I am currently working as a Postgraduate Researcher at the University of Leeds, where I am actively involved in research activities. Prior to this, I successfully completed my master's degree through the renowned Erasmus Mundus joint program, specializing in Tribology and Bachelor's degree in Mechanical Engineering from VTU in Belgaum, India. Further I handle the social media pages for Tribonet and I have my youtube channel Tribo Geek.
Bio-tribological Advancements in Fixation interface of a Joint Implant
Table of Contents
Introduction
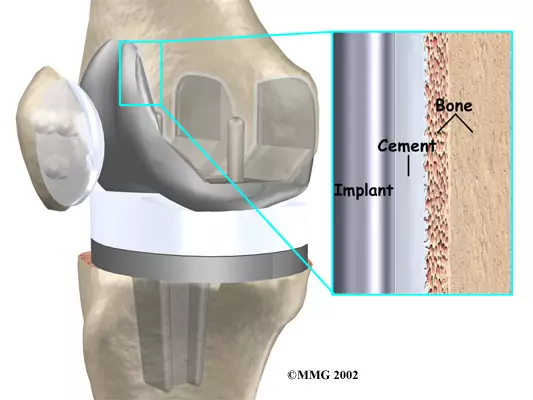
Artificial joints are typically secured using either bone cement or biological fixation. Cemented fixation, achieved with fast-drying bone cement, is commonly used for immediate fixation, particularly in knee joints. However, it faces challenges such as fretting, fatigue wear, and potential long-term stability issues. Biological fixation, relying on a textured or porous prosthesis, theoretically offers reliable long-term fixation by allowing bone ingrowth. It is prevalent in hip replacements, reducing prosthesis loosening rates, but concerns persist about aseptic loosening. Clinical issues, including sinking and prosthesis breakage, have been observed. The choice between cemented and cementless fixation remains a debated topic.
Important factors
Several factors significantly influence the stability of the interface fixation. The mechanical disparity between metal and natural bone tissue results in strain differences, leading to stress concentration and micro-motion. Appropriate micro-motion facilitates bone tissue formation, while excessive micro-motion causes the formation of fiber. A smaller interface gap decreases peri-implant tissue formation, bone-implant binding rate, and fixation strength. Besides porous materials, factors like stiffness, porous structure, topography, and keel or peg design are crucial in determining the fixation of a cementless component. Early cementless implants faced poor survivorship due to design flaws, but modern designs have shown promising results. The mechanical properties of porous implants can be tailored to match the local host bone’s stiffness, reducing bone resorption.

Fig-1 Schematic representation of mechanical damages at the articulating interface [3]
Tribological challenges
Tribological challenges are prevalent in fracture fixation components, involving crucial interactions such as biomechanical, electrochemical, and tribological effects. However, research in this area is severely limited, primarily due to the intricate in vivo environment, making the coupling mechanisms unclear. While in vitro experiments have effectively explored enhancements in material mechanical and tribological performance, there is a pressing need to further consider the in vivo biomechanical environments of fracture constructs.
Reference


Be the first to comment