I am currently working as a Postgraduate Researcher at the University of Leeds, where I am actively involved in research activities. Prior to this, I successfully completed my master's degree through the renowned Erasmus Mundus joint program, specializing in Tribology and Bachelor's degree in Mechanical Engineering from VTU in Belgaum, India. Further I handle the social media pages for Tribonet and I have my youtube channel Tribo Geek.
Bio-tribological advancements in Pressure Ulcer
Table of Contents
Introduction
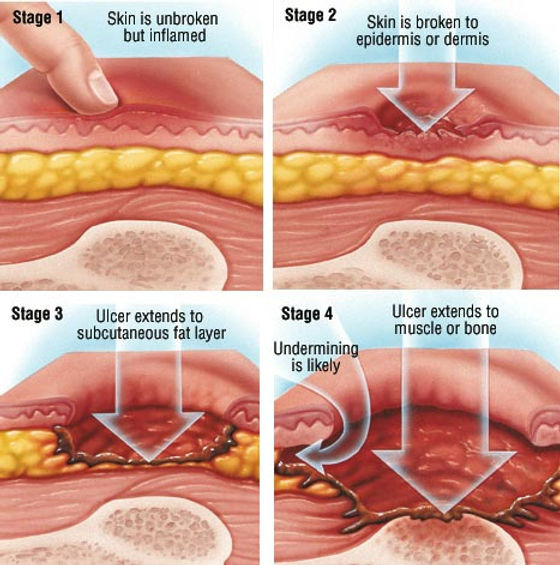
Pressure ulcers typically result from normal and/or shear pressure on the skin. Grade I or II ulcers are associated with interface shear stress, while grade III or IV ulcers may occur due to significant tissue deformation from normal pressure. Mechanical loading induces local changes in skin tissue, including local ischemia, reperfusion injury, continuous cell deformation, and lymphatic drainage, leading to tissue damage and pressure ulcer formation. Sustained pressure loading can stress the cytoskeletal structure, deform cells, and reduce tissue perfusion and lymphatic flow. This reduction in perfusion results in nutrient deficits and the accumulation of metabolic wastes, contributing to progressive tissue damage.
Mechanical Changes
The mechanism of mechanical loading-induced pathophysiological responses leading to tissue damage in pressure ulcers remains unclear. Factors influencing pressure ulcers include normal pressure loading, shear loading, surface roughness of the device interface, and microclimate. While normal pressure is considered dominant, shear loading is identified as an important factor that accelerates pressure ulcer formation. The friction coefficient of device material properties, environmental conditions, and normal load determine shear loading. Studies suggest that IL-1α cytokine expression exhibits a shear stress threshold, and patients with high-friction devices may be more prone to developing pressure ulcers. Investigations indicate that shear stress below 1.2 kPa and pressure below 2.4 kPa do not increase IL-1α cytokine concentration, suggesting these conditions may be considered safe for prolonged periods of loading.

Fig-1 Stages of Pressure Ulcer [2]
Tribological Aspect
Micro-climate and surface roughness play crucial roles in pressure ulcer development by influencing interface friction. Lower humidities generally result in a lower friction coefficient, while higher humidity levels lead to an immediate increase. Interpersonal differences in skin–device friction are linked to variations in skin hydration. Surface roughness is a significant factor, with investigations showing a minimum coefficient of friction at a Ra roughness of 4 μm for silicone surfaces against artificial skin. Minimizing interface shear stress through appropriate surface characteristics may help alleviate or prevent pressure ulcers.
Challenges and solution
Strategies to alleviate pressure ulcers primarily focus on reducing mechanical loading, particularly surface friction. Various factors are considered to reduce skin–device friction, including different materials, surface roughness, and humidity. Using alternative materials, such as foam alternatives, has been found to be more effective than standard foam mattresses in preventing pressure ulcers. Additionally, synthetic fibers have proven effective in reducing friction coefficients.
Reference
[1] https://www.lvlawny.com/post/2017/10/23/staging-of-pressure-ulcers-bed-sores
[2] https://www.verywellhealth.com/pressure-ulcer-7549469

Be the first to comment